Patients deserve the best vision from cataract surgery – this requires a quality tear film and the most stable measurements
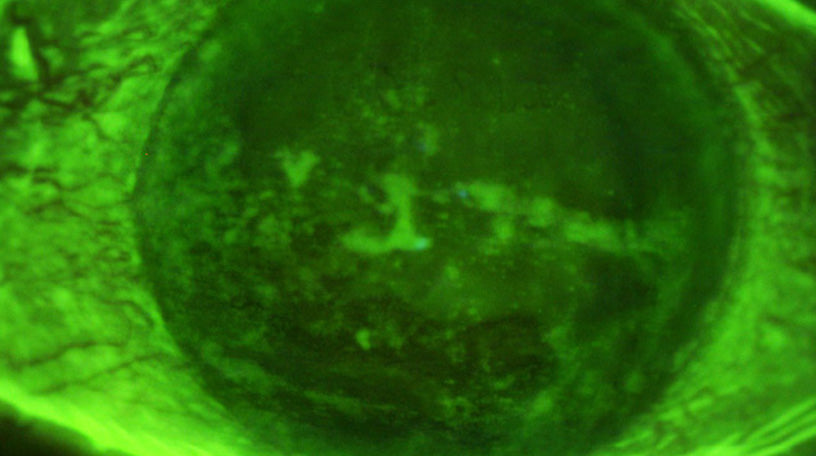
So, you are seeing a patient complaining of dry eye issues and after staining the eye with fluorescein there is extensive diffuse punctate corneal staining (Figure #1) present on the ocular surface. The patient reports increased ocular burning, gritty and scratchy discomfort, fatigue, intermittent blurring and general eye discomfort. Since the literature has shown that over 84% of dry eye is the result of meibomian gland dysfunction (MGD), you perform a quick, but detailed evaluation of the patient’s lids which shows keratinization or biofilm formation (Figure #2), plugged and reduced paste-like expression from the glands (Figure #3) and moderate redness. Your initial results support a diagnosis of MGD induced dry eye disease, but since the main reason for the examination is to obtain a new pair of glasses, you prescribe an artificial lubricant until the patient can return for a complete dry eye evaluation. However, the actual reason for the patient’s reduced vision is advanced cataracts, so treatment of the dry eye disease (DED) and MGD is even more critical to control before referring the patient for cataract refractive surgery and IOL implantation.
After examining the meibomian glands you find, in addition to the keratinization, a severe dropout of the lower lid glands (Figure #4). The two clinically significant concerns for this patient are MGD and the associated extensive corneal staining. The questions now before you are how to address and manage these co-morbid issues? Conventional wisdom suggests that you attempt to make the patient more comfortable while concurrently addressing the MGD. Initial treatment recommends a prescription of steroid QID along with hot soaks and manual lid scrubs with hypochlorous acid.
After 2 weeks of use, you see minimal, if any, objective improvement in the appearance of the corneal staining or a subjective increase in patient comfort. And, while this is concerning, you advise the patient to continue the treatment approach. Following another 3 weeks of therapy, the patient begins noticing an improvement in ocular comfort. The keratinization of the lid margin and MGD is largely unchanged, but overall progress is being made in the treatment of the cornea. And now, a follow-up examination after 2 weeks of concomitant TID steroid and BID anti-inflammatory drops produces a significant improvement in corneal and conjunctival staining.
Although corneal staining is improving, there was no change in the keratinization of the lid margin. Further, our patient reported infrequent use of hot soaks and manual lids scrubs that were earlier prescribed.


Since there had been no improvement, the patient was directed to replace their manual lid scrubs and begin one minute, once a day treatments with the NuLids System. The NuLids System is a patient administered cordless rechargeable mechanical device analogous to an electric toothbruch for the treatment of dry eye desease, blepharitis and MGD. An advantage of the NuLids System is that, depending upon the etiology of the lid disease, the cleaner/lubricant/wetting agent applied to the NuLids SoftTip can be selectively modified. For example, if Demodex in the cause of the problem, tea tree oil can be used, whereas it may be better to use hypochlorous acid for the general cleaning of the lid margins. In situations where the lids remain capped or blocked, the use of lid exfoliation and/or thermal pulsation can augment the NuLids treatment much in the same way a more aggressive in-office dental cleaning procedure is used to remove stubborn plaque as an adjunct to home brushing. Since the NuLids System oscillating Soft Tip has been proven to be both safe and effective, we anticipated similar results could occur to aid in the treatment of MGD. Shortly after making the change to NuLids, we observed that the convenience and simplicity of using this device measurably improved treatment compliance and the elimination of the patient’s many reported sysptoms. The mechanism of action of NuLids has been postulated to include:
- Cleaning bacteria as well as removing Demodex and desiccated skin from the eyelid margin,
- De-capping or opening meibomian gland orifices,
- Massaging or sonic stimulation of the lid margin mechanically breaking up stagnant meibum in the glands and improving circulation
After several weeks of mechanical stimulation of the lid margins with the NuLids System, lid hygiene had improved measurably along with a very noticeable reduction in the keratinization of the lid margins.
Additionally, there was now enough improvement in the staining of the ocular surface and the presence of a good tear film to obtain stable measurements in preparation for cataract/refractive surgery and IOL implantation.


The patient’s ocular surface and tear film quality was now stable enough to obtain the quality refractive measurements necessary for a good cataract/refractive procedure knowing that accurate measurements are a prerequisite to a good surgical outcome.
And, while the surgery gave the patient an excellent refractive result, the patient’s dry eye and MGD was exacerbated post-operatively necessitating further ongoing treatment.